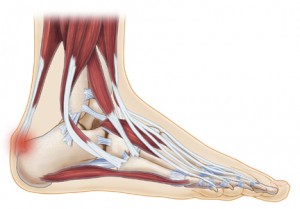
Tendons are bands of connective tissue that connect muscles to bones. The Achilles tendon runs down the back of your lower leg, connecting your calf muscle to your heel bone.
It’s the tendon that allows us to walk by raising our heel off the ground. If the Achilles tendon becomes inflamed (swollen), it’s known as Achilles tendonitis.
Generally, the inflammation is short-term, but this doesn’t mean the problem doesn’t exist. Over long periods of time, if the Achilles tendonitis is not treated it will progress into a condition known as Achilles tendonosis.
Pain develops gradually with Achilles tendonitis, but when it occurs it is described as a sharp, shooting pain, a burning pain, or a piercing pain. If left untreated, it can develop into a worse condition, and your tendon may weaken and even rupture.
Achilles Tendonitis Stages and Symptoms You Should Know About
It’s important to remember that Achilles tendonitis is a slow developing condition. In most cases, the pain is mild in the initial stages but worsens over time.
There are three stages to Achilles tendonitis, and all have their own sets of symptoms.
Peritenonitis: This is the first stage. Most people do not experience any symptoms during this initial period, but some do feel pain during activities or while resting.
Tendonosis: This is the second stage. Many times, swelling begins during this stage, as well as hard knots of tissue that begin to form on the back of the leg.
Peritenonitis with Tendonosis: This is the third stage. At this point, the tendon may partially or complete rupture and the condition can prevent ones legs from walking, and a patient may require extended recovery periods.
Other symptoms may include:
- Pain ranging from mild to severe, which may be chronic or intermittent
- Tenderness
- Mild to severe discomfort
- Stiffness
- Soreness
- Intense pain when touched
- Swelling in the lower, back part of the leg about two inches above the ankle
- Knots of tissue
What Causes Achilles Tendonitis?
Athletes are very prone to developing Achilles tendonitis, especially runners. In fact, 18 percent of serious runners experience this condition at some point in their lives. But athletes aren’t the only ones who suffer from this condition.
People who find themselves on their feet constantly or deal with stress every day may also develop Achilles tendonitis. Common causes for this condition include:
- Footwear
- Certain joint conditions such as rheumatoid arthritis and gout
- Medication side effects
- Overuse
- Aging
Improper footwear is often the cause of foot problems. In the case of Achilles tendonitis, a good example would be a woman who wears high heels for the first time in a while. The unfamiliar stretch and shortened position of the tendon can cause stress, and Achilles tendonitis can develop.
Regularly performing activities that require movement with sudden stops can also increase your risk for recurring Achilles tendonitis.
Other times, people develop this condition because they are prone to it. Some people walk abnormally, which causes their legs and feet to rotate unnaturally, which can lead to Achilles tendonitis.
Diagnosing Achilles Tendonitis – What to Expect
While diagnosing a patient for Achilles tendonitis, the usually routine steps are done first, including learning a patient’s history, giving a physical exam, measuring the passive ranges of motion of the feet, ankles and knees and by giving one or both of the following tests.
The Thompson test detects ruptures within the Achilles tendon. Usually the patient will lie face down, bending the knees as the doctor’s press on the back side of the calves. If the foot flexes, it’s a tale-tell sign the Achilles tendon is at the minimum partially undamaged.
Imaging tests may also be required. These usually involve x-rays, MRI scans, ultrasounds, or a combination of them. X-rays help detect swelling and fractures, while the MRI scan detects degenerative conditions in the tendons, and ultrasound can measure the Achilles tendon’s thickness.
Achilles Tendonitis Treatment Options For You
The first thing your doctor will consider before any treatment is attempted is the stage of the condition. If Achilles tendonitis is in its earliest stages (when there is sudden inflammation), he or she may recommend the following treatment options:
- Stop participating in the activity that caused the condition
- Place ice on the tendon for 20 minutes every waking hour for the first day or two. Heat can also be used to relieve pain and discomfort if desired
- Take medications such as ibuprofen to reduce pain and swelling
- Orthotic devices may be prescribed
- Night splints may help continuously stretch the Achilles tendon while sleeping
- Physical therapy may include strengthening exercise, stretching, and soft-tissue massage/mobilization
Common exercises to help you warm up and cool down include the:
- Achilles Tendon Stretch: While standing on a step (such as on a staircase), slowly lower your heel down over the edge of the step as you relax your calf muscles. Hold for about 15 to 20 seconds then tighten your calf muscle to bring your heel back up to the level of the step. Repeat 4 times.
- Calf Stretch: While standing in front of a wall, lean forward with one knee straight and the heel on the ground. Place the other leg in front on you with the knee bent. Push your hips toward the wall for a period of 10 seconds to stretch the calf muscle and heel cord. You should be able to feel the calf muscle stretching. Doctors recommend repeating this exercise 20 times for each foot.
Surgery is usually used as a treatment option when all other non-surgical approaches fail to restore the tendon back to its normal condition or when symptoms are severe. Surgery allows the surgeon to repair the damaged tendon.
Patients who receive surgical treatment for a torn tendon typically need three to sixmonths of recovery from surgery.
Can Achilles Tendonitis Be Prevented?
Here are some preventive tips to help you avoid developing Achilles tendonitis:
- Slowly ease into your workouts
- Warm up and cool down after exercising
- Use orthotics such as heel lifts in your athletic shoes to relieve pressure on your heels
- Wear shoes that fit properly and are appropriate for your activity
- Replace old, worn out shoes and sports equipment
- Avoid running on hard surfaces such as concrete. Instead, try dirt, grass, or wood
The best way to prevent an Achilles tendon injury from worsening isnot to ignore the problem. If you injure this tendon, see a podiatrist or your primary care physician to begin treatment. This can prevent further complications such as immobilization and extended recovery time.
Talking to Your Doctor
Here are some questions you may want to ask your doctor about Achilles tendonitis:
- What stage is my condition in?
- Will this become a chronic problem for me?
- When will I be able to return to my normal activities?
- Which warm up exercises do you recommend?
- Which over-the-counter orthotics do you recommend?
- Based on my condition, what is the long-term prognosis?




