The term neuroma was once used to describe any type of tumor composed of nerve cells, but neuromas are not tumors at all.
Neuroma refers to inflammation of a nerve and can develop in any nerve throughout the body. Neuroma commonly forms on the ball of the foot, between the metatarsal bones.
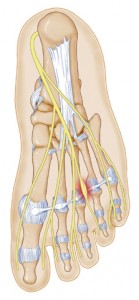
Metatarsal bones are the long bones behind the phalanges (toes), and they can be felt easily on the dorsum (top) of the foot.
There are nerves that pass between all adjacent metatarsal bones, and at the base of the toes they split into a ‘Y’ shape, where they enter the sides of the two adjacent toes.
When the nerve in between the metatarsal bones is pinched or irritated, a neuroma can result. When a neuroma forms between the third and fourth metatarsals, it is called a Morton’s neuroma.
Although this is the most common location for an intermetatarsal neuroma, this pathology does occur in between other metatarsal bones, and in each location the neuroma has a specific name.
Why Did I Develop Neuroma?
Neuromas can develop in a variety of ways. Anything that can possibly compress or irritate the nerves can lead to neuroma.
One of the most common causes of neuroma formation is footwear with a small toe box that pushes the toes together, such as high heels. Other potential causes of a neuroma include:
- Congenital or traumatic foot deformities that cause metatarsal bones to be closer together
- Injury or trauma to the foot
- Activities like high-impact sports that require repetitive movements on the balls of the feet
Neuroma Symptoms To Watch For
If you are suffering from a neuroma, understand that some symptoms do not show themselves until the condition worsens. Some common early symptoms include:
- Pain when bearing weight, and a sensation like stepping on a rock or marble
- Tingling in two adjacent toes
- Burning sensation in two adjacent toes
- Numbness of two adjacent toes
- Splaying of two adjacent toes
Symptoms of a neuroma can develop slowly, and tend to affect two toes at a time. At first, the symptoms may seem temporary—that is, they may appear only when wearing a particular pair of shoes or while performing certain activities.
Often a quick massage or disuse of the aggravating shoes will ease the symptoms or make them disappear altogether.
As time passes, however, the symptoms will last longer and longer. If the neuroma is left untreated, the symptoms can become very intense, and the nerve can be permanently damaged.
Diagnosing Neuroma – What to Expect At Your Doctor’s Office
Your foot doctor will begin your exam with questions about your medical history, daily activities, and symptoms you are experiencing. He or she will also perform a physical examination of your foot.
Your doctor will try to manipulate your foot in order to replicate the symptoms of your neuroma by squeezing the intermetatarsal area.
Often the clinical exam will be diagnostic, as the clinician will be able to feel the neuroma while they palpate and manipulate the area.
Your doctor may also ask to you put weight on the affected foot in order to see if there is clear splaying of the affected toes. Other times imaging tests may be needed in order to make a diagnosis.
A simple x-ray can reveal the proximity of the metatarsal bones, enabling your doctor to see whether the nerve is being compressed by the two adjacent metatarsal bones.
Other times, an MRI or ultrasound will be needed to visualize the neuroma. If you are experiencing any of the symptoms listed above, you should not wait to seek medical attention.
How Is Neuroma Treated?
After your diagnosis, your foot doctor will develop a treatment plan for you. Depending on the severity of the neuroma and the risks involved, he or she may use one of the following treatment options to rid you of the problem:
- Icing the area to reduce swelling
- Padding techniques to support the metatarsal arch, decrease compression, and minimize pressure placed on the nerve
- Orthotics with built-in neuroma pads
- Disuse of particular footwear that is tight in the toe box
- Avoiding activities that further aggravate the neuroma
- Anti-inflammatory medications
- Injection therapy, including cortisone or alcohol sclerosing agents
- Radiofrequency ablation (neurolysis)
If a patient does not obtain relief from one of these treatment options, surgery may be considered as a last resort. Chemical destruction of the nerve involves multiple weekly or biweekly injections of ethanol mixed with a local anesthetic.
Chemical nerve destruction has become a popular treatment option in recent years. Only your doctor will be able to assess your symptoms and decide upon the correct treatment plan for you.
You should be aware that neuromas have a high recurrence whether treated conservatively or removed surgically. You will therefore likely need to make lifestyle or footwear changes to prevent another neuroma from recurring.
Neuroma surgery involves removing a benign tumor from the nerve that innervates two adjacent toes. The procedure should only be performed in an operating room, where an anesthesiologist can monitor the patient.
During the procedure, a tourniquet is wrapped around the ankle to prevent bleeding and allow for clear visualization of the structures.
An incision can be made dorsally or plantarly (above or below) over the intermetatarsal area, after which the neuroma is identified and severed as far back into the arch as possible, prior to severing the branches to the appropriate digits.
The skin is then closed with sutures, which can be removed within two to three weeks, depending on the placement of the surgical incision. In most cases, healing is complete without complications approximately three weeks after surgery.
Following the procedure, your ability to walk will depend on the placement of the incision. A light bandage will be applied to the area, which should be kept clean and dry until your next appointment with your doctor.
Once your sutures are removed, you will be allowed to shower as usual. You must keep your foot elevated as much as possible in order to prevent swelling, and use ice throughout the first week.
Your doctor may also prescribe narcotics or anti-inflammatories to control your discomfort. You should be able to resume your normal activities within three to four weeks after the procedure, but vigorous activities should be avoided for up to two months.
If you have undergone surgery to correct a neuroma, contact your doctor immediately if:
- There is excessive bleeding within the first twenty-four hours after surgery (a little blood is to be expected)
- Pain, swelling, redness, draining in excess of what is expected
- You develop signs of infection—fever, chills, night sweats, nausea, vomiting, or general ill feeling
- Drugs prescribed are causing side effects
- New, unexplained symptoms appear, such as chest pain or shortness of breath
Complications of surgery may include:
- Excessive bleeding and hematoma formation
- Surgical wound infection
- Non-healing wound
- Numbness in toes due to cut nerve
- Recurrence or stump neuroma
Talking to Your Doctor
Here are some questions to ask your doctor about neuroma and Morton’s neuroma:
- How long should I wait if symptoms do not disappear or reappear?
- Based on the structure of my foot, what type of shoes should I be wearing to give my feet more room?
- What type of exercises should I be doing each day/week?
- What new symptoms can develop from the treatment options?
- What type of orthotics would benefit me most?




