Hallux Rigidus is a disorder that affects the first metatarsophalangeal joint (MTP), located at the base of the big toe.
Hallux refers to the big toe, and rigidus describes the stiffness or inability to move it associated with this condition.
This progressive condition is just one form of degenerative arthritis that results from wear and tear, and it can lead to immobility over time. In all joints, including the MTP joint, the ends of bones are covered by smooth articular cartilage.
When this cartilage is worn down, the bones begin to rub together. This friction causes bone spurs and other overgrowths to form on top of the bone. This overgrowth prevents the toe from bending as much as it needs to for you to walk normally.
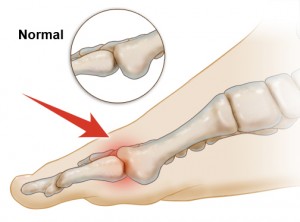
Many people confuse hallux rigidus with bunions due to their location at the base of the big toe and the fact that both affect the MTP joint.
The difference is that with hallux rigidus, the toe’s motion decreases over time. Most people who develop hallux rigidus are between the ages of 30 and 60.
Symptoms of Hallux Rigidus to Watch For
During the early stages, symptoms of hallux rigidus may include:
- Pain and stiffness in the big toe while in motion
- Pain and stiffness during cold temperatures
- Swelling around the joint
- Difficulty bending big toe up and down
- Difficulty walking, running, or squatting
- Bone spurs or other types of overgrowths
- Unwanted change in gait
As the condition progresses and worsens, symptoms may include:
- Pain, even while resting
- Difficulty wearing shoes due to bone spurs that have developed
- Pain in other parts of your body due to a change in your gait
- Limping
What Causes Hallux Rigidus?
Hallux rigidus is usually caused by an abnormality in the anatomy of the foot. It can be a functional or structural abnormality. For example, those who suffer from flat feet or excessive pronation have defects that affect the function of the foot and big toe.
This abnormality contributes to hallux rigidus. Athletes and other people who overuse their feet, especially the big toe, can also develop this condition.
Hallux rigidus can also be caused by inflammatory diseases such as rheumatoid arthritis or gout, by injuries to the big toe, or by genetics.
How Is Hallux Rigidus Diagnosed?
Doctors would rather see a patient while they are still in the early stages of this condition. Hallux rigidus is much easier to treat if it is caught early, so if you are experiencing symptoms, you should see a podiatrist as soon as possible.
Once bone spurs develop, the condition is much harder to manage.
Your doctor will examine your foot to determine its range of motion. Imaging tests such as x-rays and MRIs (magnetic resonance imaging) may be used to determine the severity of arthritis and evaluate the overall integrity of the foot bones and joints, as other abnormalities may have developed during the early and middle stages of the condition.
Your doctor will also want to ask you about your medical and family history.
Diagnosis is made on a grading scale of 0–4, according to a classification system based on your range of motion and the results of your radiographic examination.
Normally our toe joints have approximately 75 degrees of dorsiflexion (upward motion) and 25 degrees of plantarflexion (downward motion). Here’s a look at what each grade means:
Grade 0: Dorsiflexion motion is limited to 40–60 degrees. Typically there is no pain and radiographic results are normal, although there is a 20 percent loss of normal motion.
Grade 1: Dorsiflexion motion is limited 30–40 degrees. Typically overgrowths are found on top of the foot, but there are barely any other joint changes.
Grade 2: Dorsiflexion motion is limited to 10–30 degrees. Typically there is only mild flattening of the MTP joint, mild to moderate joint narrowing, and dorsal, lateral, and/or medial bony overgrowths.
Grade 3: Dorsiflexion and plantarflexion motions are limited to less than 10 degrees each. Typically radiographs show severe changes with enlarged cysts or erosions with irregular sesamoids. Patients are in constant moderate to severe pain.
Grade 4: Typically the joint is stiff and cannot bend. Radiographs show fragments of cartilage and underlying bone that have detached from the articular surface.
Depending on the severity of your condition or the grade you receive, your doctor will work with you to create an appropriate treatment plan.
How Is Hallux Rigidus Treated?
The first thing your doctor will want to do is treat the symptoms. This can be done with a number of non-surgical methods, such as changing your footwear or modifying it by stiffening the sole or using orthotics such as an arch support.
Medications can be prescribed to reduce swelling and pain. These options work best if the condition is in the early stages or is considered mild.
If your condition is moderate or has developed into its later stages, your doctor may recommend physical therapy or injection therapy.
Injection therapy involves injections of corticosteroids that reduce inflammation and pain. If your condition is severe or in its later stages, surgery may be necessary.
Common surgeries may include:
Arthrodesis: This procedure fuses the joints if the cartilage is severely damaged or deteriorated. Damaged cartilage is removed and the joint is fixed into a permanent position by pins, screws, and/or a plate.
This allows the bones to fuse together, which eliminates the painful joint. This surgery does not allow you to bend your toe at all, but it is permanent, very strong, and will withstand vigorous activity. Walking boots are worn for up to six weeks after this surgery.
Arthroplasty: This procedure removes the joint surfaces and implants an artificial joint. Patients who undergo this surgery are usually older, suffer from advanced degenerative disease, and place few functional demands on their feet. This procedure may relieve the pain and preserve joint function.
Cheilectomy: If the cartilage damage is not severe, this surgery is recommended. Doctors make an incision at the top of your foot and remove the bone spurs. Swelling of the surgical site may remain for a few months after the operation, and you will be required to wear a post-operative surgical shoe for a minimum of two weeks after surgery.
This surgery is typically successful, and most patients experience long-term relief.
After your surgery, your doctor will use either non absorbable or absorbable sutures to close the incision. If your doctor uses non absorbable sutures, they will typically be removed ten to fourteen days after surgery.
If your doctor uses absorbable sutures, they will dissolve on their own. Your doctor will schedule you for a follow-up visit when x-rays will be taken and examined to see how the healing process is going.
Who’s At Risk for Hallux Rigidus?
For reasons still unknown, hallux rigidus seems to affect people between the ages of 30 and 60, and males twice as often as females. Athletes are also susceptible to this condition due to the repetitive movements required by most sports and their tendency to overuse their feet and toes.
Some people are more prone to this hallux rigidus due to heredity. If members of your family suffer from hallux rigidus, this may indicate that someday you will too. This is another reason why it’s important to see a podiatrist or other foot specialist for regular check-ups, not just when your feet hurt.
Hallux rigidus can also be caused by trauma or an injury. Most people are susceptible to toe and foot injuries, simply because we use our feet to get around. Anyone who wears improper footwear or walks barefoot, especially on hard surfaces such as concrete, is more likely to develop this condition.
Talking to Your Doctor
Here are some questions you may want to ask your doctor about hallux rigidus:
- Based on the severity of my case, how long will it be before I can resume my normal activities?
- How soon can I begin stretches and exercises?
- After treatment, what symptoms should I watch for that may indicate the problem has not been solved?
- Can you show me exactly which joint were talking about on the x-ray, then on my foot?
- If I’m young now, should I expect this to recur when I’m older?




