Tarsal coalition is an uncommon, congenital condition of the tarsal bones in the foot. It’s estimated that anywhere from 1 to 3 percent of the population have this condition, which is typically diagnosed in children and adolescents.
In tarsal coalition, two or more bones in the heel or the midfoot do not separate properly during fetal development, which can lead to a painful, flat foot. In about half of all cases, both feet are affected.
What Is Tarsal Coalition?
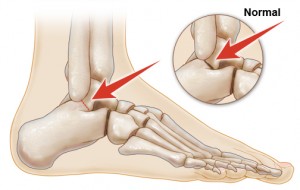
Tarsal coalition affects the bones in the midfoot and heel, which are called the tarsal bones. There are several different forms of tarsal coalition.
Any of the seven tarsal bones could be affected, but the calcaneus, navicular, and talus bones are the ones most commonly involved. In some cases, more than one type of tarsal coalition may be present in the same foot.
- Calcaneonavicular coalition (or calcaneonavicular bar): This form of tarsal coalition involves the calcaneus bone (the heel bone) and the navicular bone (located at the top of the midfoot). The calcaneus, which is the largest bone in the foot, is not completely separated from the navicular bone. This condition is sometimes called calcaneonavicular bar because the tissue connecting the two bones may appear as a “bar” between them. The exact nature of the connection can vary from case to case, however, and it could be composed of bone, cartilage, or fibrous tissue.
- Talocalcaneal coalition (or talocalcaneal bar): In this form of tarsal coalition, the calcaneus bone and the talus bone (the ankle bone) are involved. As in calcaneonavicular coalition, the connection between the calcaneus and the talus could be partial or complete, and could be made of bone, cartilage, or fibrous tissue.
- Calcaneocuboid coalition, talonavicular coalition, and cubonavicular coalition: Calcaneocuboid coalition involves the calcaneus and the cuboid (located on the bottom of the foot) bones; talonavicular coalition involves the talus and the navicular bones; and cubonavicular coalition involves the cuboid and navicular bones. These forms of tarsal coalition are very rare.
Who Is At Risk For Tarsal Coalition?
Tarsal coalition is congenital, meaning that children are born with it. While it does seem to run in families, no gene has been identified that is associated with the condition. It is believed that tarsal coalition is a result of a mutation during fetal development, so there is no way to prevent it.
What Are The Symptoms Of Tarsal Coalition?
The symptoms of a tarsal coalition can include stiffness and pain in the foot. There may also be a decrease in range of motion, depending on what type of tarsal coalition is present.
The pain typically appears in the area of the fibula, on the outside of the foot where the ankle meets the foot. Pain may also be felt on the top of the foot, and some people experience muscle spams.
In some instances, especially in some cases of talonavicular coalitions, there may not be any symptoms at all. Symptoms may be more pronounced if the tarsal coalition has ossified (i.e., new bone growth has appeared).
How Is Tarsal Coalition Diagnosed?
Patients may first seek treatment when they have pain or stiffness in the affected foot. In some cases, symptoms are precipitated by a recent weight gain, a new athletic activity, or an injury. In adolescents, tarsal coalition is sometimes discovered because their bones are ossifying.
The new rigidity may bring on pain and stiffness in the foot, prompting an investigation.
A physical exam by a podiatrist, orthopedist, or other healthcare professional may help pinpoint the location of the pain, and may also reveal a lack of motion in the heel area. When tarsal coalition is suspected, imaging studies may be done to locate the source of the pain and the location of the coalition.
- X-Ray: A plain x-ray may show some forms of tarsal coalition, X-rays may be taken of the top of the foot (anteroposterior), from an angled side view (internal or medial oblique), and a straight side view (lateral). Calcaneonavicular and talonavicular coalitions can usually be seen on a plain x-ray.
- CT (computed tomography) scan: A CT scan is the best way to visualize and diagnose a tarsal coalition. A CT scan may be performed if x-rays don’t show the suspected source of the symptoms, or if an x-ray does not provide a good view of the tarsal coalition. CT scans may also used prior to surgery, in order to determine more accurately the location of the bone or tissue involved in the coalition. In particular, talocalcaneal coalition may be better seen on a CT scan than an x-ray, and most forms of tarsal coalition can be seen with CT.
- Magnetic resonance imaging (MRI): In some cases, MRI imaging may also be employed to visualize a tarsal coalition. When the coalition is composed of tissue instead of bone, an MRI will show a more complete view than an x-ray or a CT scan. A tarsal coalition can also be discovered through an MRI or other imaging test that was ordered for a completely different problem.
How Is Tarsal Coalition Treated?
- NSAIDs (non-steroidal anti-inflammatory drugs): Pain and inflammation in the foot can be treated with over-the-counter or prescription painkillers, such as NSAIDs. This is a comfort measure, and not a long-term solution for treating a tarsal coalition.
- Orthotics: In most cases of tarsal coalition, treatment is started conservatively, with bracing and orthotics. If there is pain and inflammation, the foot and ankle may be immobilized in a brace for anywhere from two weeks to a month. This can help the joints in the foot by taking pressure off them while walking, enabling them to heal. When inflammation has resolved, the patient may be fitted for special orthotics. Orthotics are worn inside the shoe, and help put the foot in a more natural position that can reduce the pain and prevent further irritation of the area of the tarsal coalition. In some cases orthotics may be enough to resolve symptoms in the long term, but if not, surgery could be an option.
- Surgery: If orthotics do not resolve the pain and stiffness, surgery may be considered. With surgery, either the “bar” connecting the bones is removed or the bones are actually fused together.
- Excision surgery: In this type of surgery, the connecting tissue between the bones is removed, and replaced with muscle or fat tissue. The muscle or fat forms a physical barrier that prevents the bones from connecting again. This type of surgery is generally very successful in calcaneonavicular coalition. After surgery, the foot is placed in a cast or a brace, and weight-bearing activity can generally be resumed within a few days.
- Fusion surgery: In cases in which excision would not be successful, such as where the tarsal coalition is too extensive, surgery may be performed to fuse the bones together. It may also be done when there is damage to the joints, when the patient is older, or if prior excision surgery was not successful. The joints in the foot are normally covered with cartilage, and during fusion surgery this cartilage is removed, which allows the bones to grow together. The bones may be held in place with pins or screws while they heal. The foot and ankle are put in a cast or a brace, and weight-bearing activity is suspended for anywhere from six weeks to two months.
The success of either type of surgery is usually monitored with follow-up x-ray or MRI imaging.
What Are The Complications Of Tarsal Coalition
In some cases, a tarsal coalition is treated with rest and orthotics, and symptoms never recur. Sometimes an untreated tarsal coalition may advance, causing pain and becoming too significant for surgical excision. Furthermore, other joints may become involved and become arthritic from overuse. In these cases, fusion surgery may be used to relieve symptoms.
Children who experience pain from tarsal coalition may seek to avoid physical activity that causes them pain. They may also experience more injuries, such as ankle sprains, and may suffer from degenerative joint disease of nearby joints. A tarsal coalition will not affect the growth pattern of a child or adolescent.




