Fasciotomy of the foot is warranted if you have compartment syndrome—a painful condition usually caused by a severe injury such as foot fracture, or by an overuse injury from athletic exertion.
The syndrome occurs when pressure within the muscles builds to dangerous levels. Pressure on the muscles can decrease blood flow to nerve and muscle cells, interfering with the necessary delivery of nourishment and oxygen to the area.
Chronic compartment syndrome is usually not a medical emergency. Acute compartment syndrome, on the other hand, is considered a medical emergency that requires a type of surgery called a fasciotomy in order to prevent permanent muscle damage.
The goal of surgery is to relieve tension and pain.
Most people who have undergone fasciotomy require some type of rehabilitation therapy, depending on the cause of the compartment syndrome and the state of the soft tissue after surgery.
Fasciotomy has a high success rate, but compartment syndrome can sometimes recur. Going back to work after fasciotomy of the foot can be a challenge if your job requires long periods of standing or walking. For some people, this may mean being reassigned to a new position, or even changing jobs.
When Is Fasciotomy Appropriate?
A diagnosis of acute compartment syndrome requires immediate fasciotomy to relieve pressure and decrease the risk of tissue injury and death.
Progressive pain, numbness in toes, and decreased range of motion are classic symptoms of acute compartment syndrome, although in some cases these symptoms may be related to an accompanying foot fracture or injury.
Findings specific to acute compartment syndrome of the foot include:
- Increased pain when the toes, or metatarsophalangeal joints, are flexed
- Weak or absent pulses
- Tense tissue bulging
- Elevated compartmental pressures
- Bleeding and edema within a muscle compartment surrounded by fascia (connective tissue) and bone
Fasciotomy may be considered in patients with overuse injuries when conservative treatment measures have failed to relieve pain or improve function—for example, in severe cases of heel pain.
In chronic compartment syndrome, compartmental pressure rises and falls with activity—symptoms of pain and cramping occur during exercise and subside after exercise. Opening the fascia allows the muscle to expand, improving circulation and decreasing pressure.
Preparing for Fasciotomy of the Foot
In the case of acute compartment syndrome, you may not have time to prepare for fasciotomy. If you are undergoing fasciotomy because of chronic compartment syndrome, then preparation for surgery will be similar to preparation for any other orthopedic surgery.
Because fasciotomy requires general or regional anesthesia, you will be asked to fast and drink only clear liquids for at least six hours before the procedure. Your doctor will review your medical history and let you know whether any of the medications you are taking should be temporarily discontinued.
The Fasciotomy Procedure
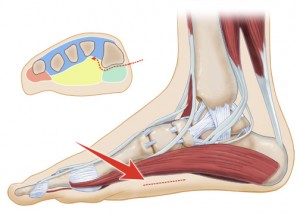
During fasciotomy, your surgeon will make incisions through the skin over the affected compartment, down to the connective tissue (fascia) surrounding the muscles and the fascia is dissected to release the muscle.
This must be done carefully to avoid damaging the nerves and blood vessels in the area. The type of incision made depends on the extent of the pressure, and the procedure may involve multiple small incisions in the skin and fascia, or long continuous incisions over the entire compartment.
In acute compartment syndrome, the wounds may be left open and covered with wet sterile dressings to allow the muscle to swell up and out of the skin. This should relieve compartmental pressure and subsequently restore circulation and decrease swelling.
When performed in a timely fashion, fasciotomy can decrease pain and restore muscle function. The wounds may be allowed to close by secondary intention (on their own) or your surgeon may close them with sutures. In some cases, skin grafting may be required.
During surgery for chronic compartment syndrome, the fascia will be left open but the overlying layers of tissue and skin will be closed with sutures. Plantar fasciotomy, for example, can be performed by making two small incisions on either side of the heel.
Using an endoscope inserted in one incision for guidance, your surgeon will dissect the fascia near the heel through the other incision. The incisions are then closed. As the wound heals, new fascia will grow to connect the opened portion. This lengthens the tissue around the muscle and relieves pressure.
Compartment pressure readings are monitored during and after the procedure.
After Fasciotomy Surgery
For patients treated with fasciotomy for acute compartment syndrome, proper skin care is essential. An ankle-foot orthotic is often needed. You may be referred to a physical therapist for gentle range-of-motion exercises to prevent contractures.
Exercises to strengthen muscles and gait training with an assistive device are other measures that may be required to improve function. If you continue to have problems performing ordinary activities, occupational therapy may be considered.
Rehabilitation for patients who undergo fasciotomy for chronic compartment syndrome involves tissue healing, muscle loading, scar tissue formation, and consideration of all tissues contained in the involved compartment.
It initially consists of protection of the affected area, rest, ice, compression, and elevation. This is followed with stretching and strengthening exercises to re-establish range of motion and soft tissue mobility and eventually enable you to resume normal activity — or if you are an athlete, to resume participation in your sport.
Return to normal function after a successful fasciotomy usually takes two to three months.
What Are The Risks of Fasciotomy of the Foot?
Fasciotomy has been associated with a variety of complications, including skin sloughing, infection, muscle weakness or damage, nerve or blood vessel injury, and scarring.
Contractures of the skin and soft tissue from either the initial procedure or secondary wound closure may also occur. Reported complications of fasciotomy with skin grafting are infection, scarring, and contracture at the donor site.
Compartment syndrome may recur in patients with excessive scar tissue or in those with inadequate initial release of the fascia.




