The surgical repair or replacement of a diseased joint is known as arthroplasty. This procedure may be considered when conservative treatments no longer provide adequate relief from joint pain and/or disability.
The joint can be repaired by resurfacing the bones or replaced with a prosthesis. Many people who have undergone arthroplasty report substantial improvement in their joint pain, which in turn improves their quality of life.
Arthroplasty is used to treat a variety of foot and ankle conditions that cause destruction of cartilage and bones, such as arthritis. In patients with arthritis, replacing an arthritic joint allows for greater range of motion, and thus less stress is transferred to adjacent joints.
This decreases the chances of arthritis developing in those joints. Arthroplasty can be a minor or major surgery, depending on what type of procedure is performed. Your surgeon will determine whether you are a suitable candidate for surgery.
When Is Arthroplasty Appropriate?
Arthroplasty may be appropriate if you have chronic joint disease, long-standing pain, or severe disability. Many factors will determine whether you a good candidate for surgery.
Regardless of the type of procedure, a recommendation for surgery is typically made only after conservative treatments have been exhausted and after you are deemed healthy enough for surgery.
However, it is ultimately up to you whether to proceed with surgery.
If you have one of the following conditions of the foot or ankle, joint repair or replacement surgery may be an option for you:
- Advanced arthritis of the ankle
- Rheumatoid arthritis
- Osteoarthritis
- Bone fracture
- Infection
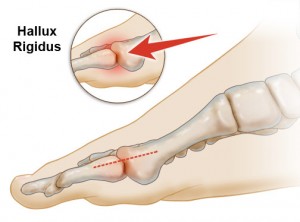
- Moderate to severe hallux rigidus (arthritis of the big toe joint)
- Previous unsuccessful bunion surgery
- Claw toes, mallet toes, or hammertoes
Preparing for Arthroplasty Surgery
To be cleared for surgery, you will need to see your primary care physician or internist for a general medical evaluation.
You will also have preoperative visits with your surgeon. You may need to take several types of tests, including blood tests, a cardiogram, a urine sample, and a chest radiograph.
The amount of preparation you need for joint repair surgery is less than for joint replacement surgery.
The latter procedure is more complex, has a higher risk of complications, involves more hospital resources, and requires a longer recuperation period. To ensure that you are adequately prepared for either surgery, make sure you:
- Understand your procedure by asking questions and voicing any concerns.
- Write down all your medical information and bring it with you to every doctor’s appointment; this includes your emergency contacts, healthcare providers, medical conditions, medications, allergies, dietary restrictions, insurance coverage, and legal arrangements.
- Stay healthy or take steps to improve your health before your surgery.
- Avoid drinking alcohol 48 hours before surgery.
- Plan for your return home: arrange for someone to pick you up from the doctor’s office or hospital and stay with you after the surgery, and make sure your home is equipped with everything you need to make your recovery as comfortable as possible.
- Follow your surgeon’s instructions for what to do in the 24 hours before surgery.
The Arthroplasty Procedure
Arthroplasty can be performed in multiple ways with varying degrees of complexity and may be done as part of another surgery. Procedures for joint replacement and joint repair are described below:
- Joint replacement
The surgical approach for joint replacement may vary. Total joint replacement for the ankle and big toe are described here:
- Ankle replacement
Ankle replacement is most often recommended for patients with advanced arthritis of the ankle, destroyed ankle joint surfaces, and an ankle condition that interferes with daily activities. The procedure is done under general anesthesia in the hospital.
Your surgeon will make an incision in the line of the tibialis anterior muscle, and then a sharp incision through the connective tissue and muscle sheath, bordering the lateral side of tendon to avoid the neurovascular bundle.
Vessels that cross the joint transversely are diathermied (burned). A retractor is used to expose the anterior tibia and the ankle joint capsule. Your surgeon will continue to cut through the tissues and bones (the medial and lateral malleoli) until the ankle joint is opened.
At this point, the goal is to remove all the damaged bone and cartilage and reshape the three remaining bones (the tibia, fibula, and talus) to accommodate the prosthetic implant. The parts of the new artificial joint are attached to the cut bony surfaces.
A special glue or bone cement may be used to hold them in place. To help support the artificial ankle, screws may be inserted through the two leg bones (the fibula and tibia). A bone graft is implanted between the ends of the fibula and tibia.
This makes your new ankle more stable. After putting the tendons and tissues back into place, your surgeon closes the wound with sutures. A splint, cast, or brace may be applied to keep the ankle from moving.
- Big toe
Patients who undergo metatarsophalangeal joint replacement for hallux rigidus will receive general or regional anesthesia. Your surgeon will make an incision in the skin over the joint and then divide the tissue and retract the tendon to expose the joint capsule.
He or she then removes the joint and clears away part of the medullary canals of the first metatarsal and proximal phalanx to accommodate the prosthetic joint implant.
A preliminary reduction with a trial implant is done to ensure a snug fit, and the implant components are then placed in each canal. After the joint capsule and incision are closed, a flexible splint is applied.
- Joint repair
Here are a few techniques used to repair joints in the foot and ankle:
- Interpositional arthroplasty
This procedure consists of removing some of the damaged bone and replacing it with a piece of soft tissue from the foot, such as tendon or capsule, between the joint to allow for some motion.
This may be an option for the patient with moderate to severe hallux rigidus, arthritis of the big toe joint. The surgery is performed under regional anesthesia. A dorsal linear incision is created just medial to the extensor hallucis longus tendon.
A sharp and blunt dissection is made, taking care to protect the neurovascular structures. The joint is exposed. Any inflamed tissue or loose bodies are removed. Tunnels are created for the new tissue. The new tissue is attached using stiches.
Before closing the incision, range of motion is tested. A light, sterile compressive dressing with toe tape (spica) is applied. Removing part of the bone shortens the big toe slightly but preserves some movement.
- Distraction arthroplasty
This technique stretches the joint apart for a while. It may be recommended for a patient who has ankle arthritis. Appropriate candidates are young active patients with arthritis, which is usually the result of an injury rather than a deformity.
The surgery is done in two stages. The first stage is the application of an external frame with wires or pins from the tibia down to the foot. The second surgery, which is done approximately three months later, is to remove the frame and apply a splint or cast dressing.
The incisions where the pins and wires are placed are very small. You may be allowed to put weight on the foot and walk and participate in physical therapy while in the frame.
- Resection arthroplasty
This procedure involves increasing joint space by removing the damaged portion of the joint. It is mainly recommended for older patients, those with severe arthritis, or those who have previously had unsuccessful bunion surgery.
Typically, surgery takes about one hour, and patients are able to go home within two hours afterwards.
After Arthroplasty Surgery
Most people have some pain after foot and ankle surgery. You will be given medication for pain at the time of surgery and a prescription for pain medication along with instructions for how to relieve pain at home.
Elevating your foot above the level of your heart for one to two weeks following surgery is usually advised.
A physical therapy regimen may be prescribed to help you regain strength in your foot or ankle and to restore range of motion. When you can resume ordinary daily activities will be determined by your doctor.
Your activities may be limited for three to four months after major surgery. You may need special shoes or braces.
Surgery can relieve joint pain and make it easier for you to perform daily activities. Full recovery can take four to nine months or more, depending on the severity of your condition before surgery and the complexity of the surgery.
Risks of Arthroplasty To Be Familiar With
The potential complications of joint repair surgery are similar to those for any type of surgery — infection, scarring, persistent pain, and surgical failure.
With distraction arthroplasty, it is common to have irritation at one of the pin or wire sites, and some patients may experience nerve pain as the frame stretches the ankle joint.
With any joint replacement surgery, the implant may loosen or fail over the years. Additional surgery may be necessary if the implant failure is severe. Other risks involved with joint replacement surgery are:
- Joint weakness, stiffness, or instability
- Skin not healing after surgery
- Nerve damage
- Blood vessel damage
- Bone break during surgery
- Dislocation of the artificial joint
- Allergic reaction to the artificial joint




